Blood types and transfusions
- Christie Roberts

- Jun 6, 2025
- 16 min read
I recently discovered that a lot of people have no idea what their blood type is, unless they've previously donated blood. I was born in Singapore and at the hospital they gave me a little card which told me that I'm A+, so I figured that was a universal experience. (but it turns out I'm just special).
But what does A+ actually mean? Let's find out!
Red blood cells have surface antigens, which act as flags to let the body recognise them as 'self' and not be attacked by the immune system. Blood types are determined by which type of antigen is present.

From the image above, we can see that one cell has an A antigen (type A), one has a B antigen (type B), one has both A and B antigens (type AB) and one has no antigen (type O).
Stick with me, because It's about to get even weirder... introducing Rhesus factor.
Rhesus (Rh) is what gives you the positive or negative after the letter. Rhesus D (RhD) is another antigen found on the surface of some cells. If RhD is present, the blood type is Rh positive. If not, it's Rh negative. The image above shows only cells with no RhD, so these would all be negative blood types. The image below shows positive blood types, with RhD present.

Therefore a cell with A antigens, B antigens and a RhD antigen would be an AB+ blood type. This adds a level of complexity when it comes to blood type matching for transfusions.
If you are Rh +ve, you can recieve Rh +ve or Rh -ve blood. However, if you are Rh -ve, you can only recieve Rh -ve. Put more simply, a positive blood type can receive positive or negative, but negative can only receive negative.
Along with antigens in the body, we have antibodies- these are proteins that mark non-self antigens for destruction by the immune system. This is why blood type matching for transfusions becomes important, because the antigens must match to avoid being marked for destruction by antibodies.
Type A blood cells have anti B antibodies- if a type B antigen is detected, it will be destroyed. Similarly, type B cells have anti A antibodies to destroy type A antigens. Type AB blood has no antibodies, as it has antigens for both A and B, so it would just end up destroying itself. And type O cells have anti A and anti B antibodies, as it has no antigen, so can only be matched with type O.
Negative blood types will also have anti D antigens, as they are not compatible with Rh +ve blood cells.
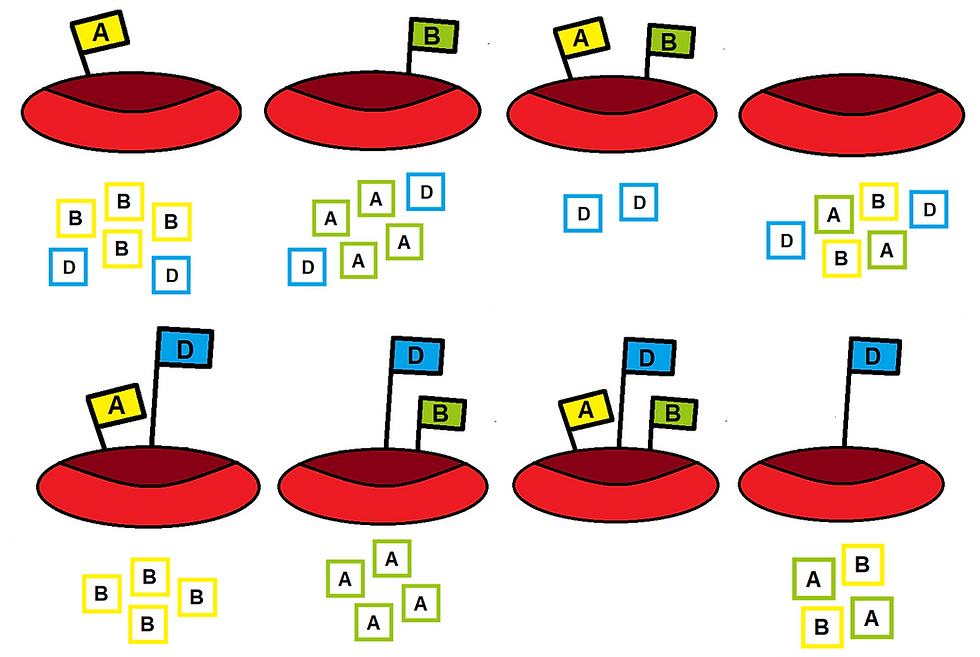
For clarification, the little boxes are the anti-antibodies. I've tried my hardest to describe this pictorially, but my artistic skills are limited and I use MS Paint to create these so please bear with.
Who can receive what?
Type O- is known as the universal donor, meaning anyone can recieve it. There are no antigens present for the body to be able to attack as foreign. Type AB+ is the universal recipient, meaning they can receive blood from anyone as there are no antibodies to attack anything.
Here's a handy dandy table to summarise who can recieve what blood:

Blood transfusions
For the purposes of the rest of this post, I'm only going to be talking about transfusions of packed red blood cells (PRBC) rather than any other blood components that can also be transfused, such as platelets, cryoprecipitate (cryo) and fresh frozen plasma (FFP).
A blood transfusion is a potentially risky procedure that should only be undertaken when clinical benefit or need outweighs risk (Oxford University Hospitals, 2012). Prior to administering blood products, blood must be taken for group and save and crossmatching using an EDTA tube (purple top in my local hospital Trust, may vary). 'Group' refers to the determination of a patient's ABO and RhD status (blood type) and 'save' refers to the fact that this information is kept for a specified time period, typically 3 months, in case a transfusion is required later. However, if a transfusion has been received in the preceeding 3 months, this sample is often only valid for 72 hours (Leeds Teaching Hospitals NHS Trust, no date a; Oxford University Hospitals, 2015). The grouping test may also include testing for atypical antibodies which may be present as a result of previous transfusions or pregnancy (North West Anglia NHS Foundation Trust, no date). 'Crossmatch' refers to the process of matching donor blood to recipient blood type to ensure compatibility (Leeds Teaching Hospitals NHS Trust, no date b). If crossmatching is not available, for example in an emergency, O- blood will be issued given that this is the universal donor.
Indications for blood transfusion include massive haemorrhage where circulating volume needs to be replaced and severe anaemia- thresholds for haemoglobin may vary, but typically we transfuse at 70g/L (local reference ranges for Hb are 130-170 g/L for males, 120-165 g/L for females (NICE, 2015; Oxford University Hospitals, 2024)).
Many blood transfusions systems now use electronic data systems to ensure that blood can be tracked 'vein to vein' to ensure safety and traceablity of blood products (Oxford University Hospitals, 2012). 1 unit of PRBC must be transfused within 4 hours and a strict schedule of observations must be undertaken during the transfusion to monitor for potential reactions (Oxford University Hospitals, 2012). Blood pressure, temperature, pulse and respiratory rate must be recorded prior to starting the transfusion, within 15 minutes of starting, and at the end of each unit provided. Typically, acute transfusion reactions will occur within the first 30 minutes of transfusion, but these will not necessarily be severe reactions (Oxford University Hospitals, 2012).
And as a spoiler, I'm going to tell you that if something is going wrong, the answer to everything is stopping the transfusion, reporting the reaction, returning the blood to the blood bank, monitoring the patient, and taking further blood samples from the patient (Oxford University Hospitals, 2012). But read on for more specifics...
Transfusion reactions
Acute haemolytic reaction
Probably the most common transfusion reaction is an ABO incompatibility reaction. This ia a type of acute haemolytic reaction when an incompatible blood type has been administered. Incompatible blood cells will be destroyed by intravascular haemolysis. Haemolysis is defined as the rupture of red blood cells (Rout et al., 2023). Typically this will happen during the transfusion or within 24 hours after, but delayed reactions can occur between 14 to 30 days after transfusion (Rout et al., 2023). The attack can work both ways- with recipient antibodies targeting donor RBCs (known as major incompatibility) or with donor antibodies attacking recipient RBCs (minor incompatibility) (Rout et al., 2023).
A classical (but rarely so neatly packaged) triad of symptoms for an acute haemolytic reaction is fever, flank pain and haemogloburia (Rout et al., 2023). But we do not live in a perfect world, so other signs and symptoms may include tachycardia, chills, rigours, dyspnoea, chest pain, pain at infusion site, a sense of impending doom, (always fun) and hypotension (Lifeblood, no date a).
Renal dysfunction and failure are later signs (Rout et al, 2023), along with DIC. Disseminated Intravascular Coagulation is a rare but serious possible result of ABO incompatibility resulting from profound intravascular haemolysis (Streiff, 2023) and is associated with a mortality rate ranging from 20 to 50% (Papageorgiou et al., 2018).
Management involves assessing the patient for signs of a haemolysis reaction (good luck with that wide range of symptoms), stopping the transfusion, checking ABO compatibility of the patient blood group and transfused unit, and supportive management of symptoms (Lifeblood, no date a). Aggressive hydration and diuresis should be provided (unless contraindicated for volume overload) to reduce the effects of free haemoglobin in the bloodstream, which can contribute to DIC and renal failure (Lifeblood, no date a; Rout et al., 2023). Blood should be returned to the lab to be retested, along with the patients blood to assess for haemolysis (Rout et al., 2023). Additionally, urine sould be saved for testing if there are signs of haemolysis and haemoglobinuria (Oxford University Hospitals, 2012). P.S haemoglobinuria is different from haematuria.
Most ABO incompatibility reactons are preventable by minimising human error through checking blood products and ensuring accurate grouping and crossmatching, however there can be unavoidable unidentified immune incompatibility (Rout et al., 2023).
Febrile non-haemolytic reaction
This is thought to arise from accumulation of cytokines (signalling messengers in the immune system) released by donor blood leukocytes during storage of blood products (Lifeblood, no date b). Occurs more commonly in platelet transfusions, but can and does happen with PRBCs too (Heddle, 1999).
The main symptom is a temperature increase of 1deg above baseline, or to above 38deg, which is uaually an isolated finding and this temperture increase will typically occur in the first 15 minutes of starting a transfusion. However, fever can be associated with many other transfusion reactions so this should be a diagnosis of exclusion (Lifeblood, no date b) when haemolysis reactions and septic reactions have been ruled out. There may be other inflammatory symptoms associated, such as myalgia, headache and rigours (JPAC, no date a; Lifeblood, no date b).
Febrile reactions have become less common since introducing leucodepleted blood components, which is considered standard practice in the UK (JPAC, no date a; JPAC, 2024).
Management is to stop transfusion (wow unbelivable) and give paracetamol to address fever. Once other transfusion reactions have been ruled out, it may be possible to restart the transfusion at a slow rate with careful monitoring (Lifeblood, no date b).
Allergic reaction
Can range from mild reactions to full on anaphylaxis when someone reacts to substances in the transfused blood. Most allergic reactions will occur within minutes of transfusion starting, with typical allergic symptoms like hives and urticaria for a mild reaction (Lifeblood, no date c) all the way through to a typical anaphylaxis picture- hypotension, bronchospasm, angiodema, shock and loss of consciousness (Lifeblood, no date d).
Mild reactions occur in 1-3% of transfusions, typically due to hypersensitivity to plasma proteins in transfused blood (Lifeblood, no date c; Suddock and Crookston, 2023). More severe reactions like haemolysis should be ruled out, but typically a mild allergic reaction will not require further investigation and management beyond pausing the infusion, administering antihistamines, and restarting at a slower rate (Lifeblood, no date c).
Potential causes of anaphylactic reactions include IgA deficient patients who have anti IgA antibodies and are then given blood containing IgA (Suddock and Crookston, 2023), antibodies to plasma proteins in transfused blood, and transfusion of an allergen to a sensitised recipient- for example if the donor had penicillin in their system and blood was given to someonw with a penicillin allergy (Lifeblood, no date d). To manage anaphylaxis, do what you would usually do. (everybody together now...) stop the transfusion, and manage the rest as usual with an A-E approach. Maintain a patent airway, administer oxygen, support blood pressure. Administer IM adrenaline initially, and consider following up with antihistamines and steroids (Lifeblood, no date d; Resuscitation Council UK, 2021).
If someone requires repeated transfusions and is repeatedly suffering with allergic reactions, washed red blood cells may be an option. This process removes some of the plasma proteins and IgA which may be causing allergic reactions (Ontario Regional Blood Coordinating Network, 2017). Washing can remove 90-95% of plasma proteins but the method of washing will affect the proportion of units that end up being equivalent to IgA deficient (Cardigan et al., 2020).
Transfusion Associated Circulatory Overload (TACO)
TACO (phenomenal acronym) is defined as acute respiratory distress and pulmonary oedema in the 12 hours following a transfusion due to hypervolaemia (SHOT, 2024). It typically will occur in patients receiving large volumes of transfused products over a short time period, but can also easily occur in patients receiving small volume transfusion if they have existing risk factors such as congestive heart failure, pulmonary oedema, or renal impairment (JPAC, no date b; SHOT, 2023; Tobian, 2025a).
The International Society of Blood Transfusion (2018) have diagnostic criteria- A total of 3 criteria including either A or B is diagnostic of TACO:
A- Acute or worsening respiratory compromise- dyspnoea, tachypnoea, oxygen desaturation, cyanosis
B- Acute or worsening pulmonary oedema
C- Cardiovascular system changes- hypertension, widened pulse pressure, venous jugular distension, tachucardia, peripheral oedema
D- Evidence of fluid overload- positive fluid balance, response to diuretic therapy/dialysis, changes in weight
E- Relevant biomarkers eg an increase in BNP
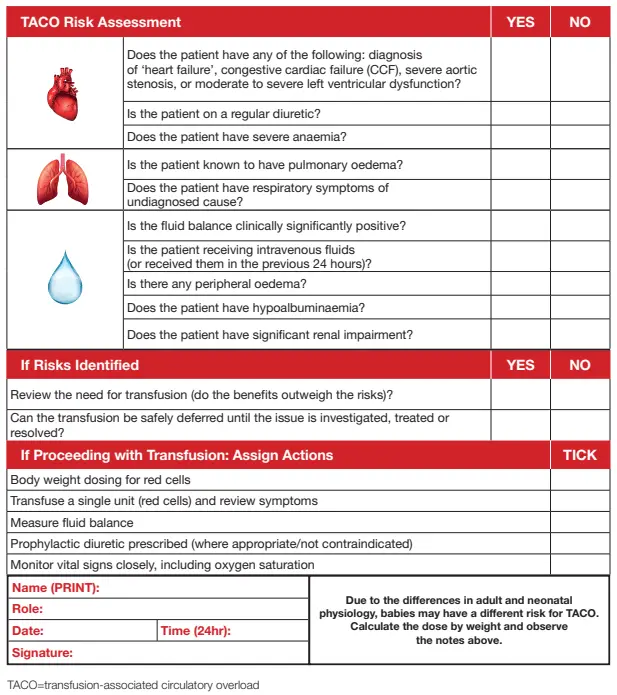
All patients should be risk assessed for TACO prior to transfusion, using this tool by SHOT (2023)- you're gonna have to zoom in, sorry..
The assessment looks at presence of risk factors and ways to mitigate them if blood transfusion remains necessary. This includes dosing blood by mL rather than units, giving singular units then reassessing, use of diuretics (including prophylactically), monitoring of fluid balance, and slow transfusion with close monitoring of vital signs (SHOT, 2023; JPAC, no date b).
Management involves stopping the transfusion and starting supportive care- sit upright, provide supplemental oxygen and start diuretics to manage hypervolaemia (Lifeblood, no date e; Gupta and Yan, 2021). If further transfusion is clinically necessary, ensure that the preventative measures above are implemented to minimise risk.
Transfusion Related Acute Lung Injury (TRALI)
TRALI is a syndrome characterised by acute pulmonary oedema (confirmed to be non-cardiogenic, with bilateral exudative infiltrates on CXR) with hypoxia and dyspnoea, leading to respiratory failure, occurring within 6 hours of transfusion (Latham, 2016; Cho, Modi and Sharma, 2023). Other symptoms may include pyrexia, tachycardia, tachypnoea and hypotension (Lifeblood, no date f).
Pathogenesis remains somewhat unclear, but human leucocyte antigen (HLA) antibodies and human neutrophil antigen (HNA) antibodies found in donor blood have been implicated, known as antibody mediated TRALI. Donor antibodies bind to recipient antigens, activating neutrophils in the lungs and causing damage and leakage to pulmonary vasculature through release of oxidases and proteases (Lifeblood, no date f; Cho, Modi and Sharma, 2023). HLA and HNA antibodies are found in the plasma, so this reaction is more common with tranfusion of FFP and cryo, or other transfusions with higher proportions of plasma (Cho, Modi and Sharma, 2023). Antibodies against HLA and HNA are formed from exposure to corresponding antigens through pregnancy, transplant, or previous transfusion in a process known as alloimmunisation (Martins et al., 2017) therefore a way to minimise antibody mediated TRALI is to use blood/plasma products from people who have not had exposure to these antigens- an example would be using male only plasma in the production of FFP or cryo (Lifeblood, no date f; Latham, 2016), and screening female donors for HLA and HNA antibodies (Cho, Modi and Sharma, 2023).
If TRALI is suspected, HLA and HNA typing of the recipient, and testing for antibodies from the donor, can help to confirm a diagnosis (Lifeblood, no date f; Latham, 2o16) so the blood bank should be informed and transfused blood returned for testing.
Management is similar to all the other transfusion reactions- stop the transfusion, and provide supportive care, including cardiovascular and respiratory support. Mechanical ventilation may be required depending on the extent of respiratory failure, but there is little evidence for use of diuretics depite pulmonary oedema (Lifeblood, no date f). However, a response to diuretics may help with a differential diagnosis of TACO (Gupta and Yan, 2021).
Graft Vs Host DIsease (GvHD)
This is something typically seen after transplants, but I guess you could argue that a blood transfusion is a type of transplant? Transfusion-associated GvHD (TA-GvHD) is a rare but very very bad reaction typically occurring 1-2 weeks post transfusion. It has an estimated mortality rate of 90-100% with very limited scope for treatment post onset- requiring a focus on prevention (Williamson, 1998; Kopolovic et al, 2015).
Symptoms include fever, rash, diarrhoea, jaundice and pancytopenia (low red cells, white cells and platelets) due to bone marrow aplasia (Lifeblood, no date g; Elmakki et al., 2023). Cause of death is usually from overwhelming infection secondary to pancytopenia (Lifeblood, no date g; Tobian, 2025b).
Typically, GvHD occurs in patients who are already immunocompromised, due to the immune system being unable to recognise T lymphocytes in transfused blood products as foreign, and the lymphocytes engrafting into the recipient's bone marrow. Donor T cells then recognise the recipient's body tissues as foreign and attack them (Lifeblood, no date g; Elmakki et al., 2023). Therefore, the degree of immunocompromise, and the number of viable T lymphocytes in the transfusion will impact on the risk of GvHD (Lifeblood, no date g). The number of T cells can be reduced by the degree of leucodepletion and irraditation, and the age of the blood being transfused- lymphocyte proliferation declines with longer storage time (Lifeblood, no date g; Australian and New Zealand Society of Blood Transfusion (ANZBST), 2024). Kopolovic et al. (2015) found that of 158 reported cases of TA-GvHD, in 93.7% the transfused product was less than 10 days old. The remaining 6.3% cases were reported as 11-14 days old, and no cases were reported beyond 14 days of storage of blood product. Due to this finding, ANZBST (2024) recommend that cells stored for 14 days can be used as an equivalent for irradiated blood product for patients at risk of GvHD when necessary.
HLA matches are also considered as a risk factor for TA-GvHD. HLA-matched blood products are those that bear immunological homogeneity between the donor and recipient. This can come from blood related donors, or simply genetic similarities (Lifeblood, no date g; Elmakki et al., 2023). In bone marrow and solid organ transplants, HLA matching is important to reduce the risk of rejection and GvHD, as they need things to engraft into the bone marrow (Imperial College Healthcare NHS Trust, 2024). However in blood transfusion, the lack of genetic diversity creates the opportunity for donor lymphocytes to avoid HLA-mediated immune detection by the recipient, with a retained ability for donor lymphocytes to react to host tissues (Kopolovic et al., 2015). Basically, there's more viable T lymphocytes available to attack things. It's therefore recommended that blood from related people, or HLA matched blood products, are irradiated prior to transfusion (ANZSBT, 2024).
As I mentioned, there really isn't any treatment available- corticosteroids and cytotoxic agents aimed at suppressing the immune system may have some effect, but the massive mortality rate remains (Lifeblood, no date g). BUT prevention is possible. This includes risk assessment of individuals receiving blood transfusions including assessing for immunocompromise, HLA matching, and use of irradiated products (although this is not necessarily practicable for all transfusions, hence risk assessment) (Lifeblood, no date g; Elmakki et al., 2023; ANZBST, 2024). However, to be the bearer of bad news, up to 50% of patients who develop TA-GvHD had no identified risk factors (Kopolovic et al., 2015). It's pretty bleak.
Transfusion complications
Not quite a reaction, but not good either. As we know, blood transfusion is an invasive procedure which carries infection risk, both bacterial and viral.
Bacterial infection
Infection can arise from bacteria on the donor's skin during blood donation (most common), unidentified and asymptomatic bacteraemia in the donor, and bacterial contamination from the environment or during preparation/thawing of blood products (Lifeblood, no date h). Bacterial contamination is more common in platelets, as these are stored at room temperature, giving bacteria a more ideal medium to proliferate (Benjamin, 2016). However, some infection can also brew in RBC donations despite cold storage, particularly if cells are stored for several weeks or if they use iron as a nutrient for growth (Lifeblood, no date h). An example of a bacteria is Yersinia enterocolitica. The mortality rate of post-transfusion sepsis due to Yersinia enterocolitica is around 54% (Guinet, Carniel and Leclercq, 2011).
Viral infection
Fortunately, viral infection from blood and blood products is uncommon nowadays due to enhanced screening processes and safer procurement methods. Unfortunately, it took tragedies to get to this point (see: UK infected blood scandal; Arkansas prison blood scandal).
In the UK, donors complete a screening assessment to establish potential risks. Some viral tests will be applied to all samples, and some will be discretionary based on personal factors such as country of birth, lifestyle factors (sex, tattoos, piercings and the like) and recent travel (NHSBT, no date). Donors are excluded if they have/had HIV, Hep B, Hep C, Human T-Lymphotrophic virus (HTLV) or syphillis, or have injected drugs. A more exhaustive list of who can and cannot donate is available here.
Tests conducted on all samples:
Treponema pallidum- responsible for syphillis, Yaws and Pinta
Hepatitis B (HBV)
Hepatitis C (HCV)
Hepatitis E (HEV)
Human Immunodeficiency Virus (HIV)
Human T-Lymphotrophic Virus (HTLV) - first time donors
Discretionary tests:
Malaria
Trypanosoma cruzi- T-cruzi
West Nile Virus (WNV)
Cytomegalovirus (CMV)
(Give Blood, no date; NHSBT, no date)
I'm not going to go into the signs and symptoms and treatments of bloodborne bacterial and viral infections, or sepsis, because frankly, I've been writing this post for too long and that's outside the scope.
Woof, that was a long one. What started as me making funny little pictures on Paint turned into me finally having to understand how antigens and antibodies work. Like the gif says- donating blood does save lives, but it's also true that there are significant potential risks from receiving donated blood. Being aware of potential reactions is step one, and knowing how to manage them is step 2... so remember kids, stop the transfusion!!!
Lots of love, Christie x
References
Australian and New Zealand Society of Blood Transfusion (2024) Guidelines for the prevention of transfusion-associated graft-versus host disease (TA-GVHD). Available at: https://anzsbt.org.au/wp-content/uploads/2024/02/TAGVHD-Guideines-2024.pdf (Accessed 04/06/2025)
Benjamin, R. (2016) 'Transfusion-related sepsis: a silent epidemic' in Blood, 127(4), pp. 380-381.
Cho, M, Modi, P, Sharma, S. (2023) Transfusion-related acute lung injury. Available at: https://www.ncbi.nlm.nih.gov/books/NBK507846/ (Accessed 04/06/2025)
Elmakki, E. et al. (2023) 'Transfusion-associated graft-versus-host disease in adults' in Cureus, 15(8).
Give Blood (no date) Tests we carry out on donated blood. Available at: https://www.blood.co.uk/the-donation-process/further-information/tests-we-carry-out/ (Accessed 04/06/2025)
Guinet, F., Carniel, E., Leclercq, A. (2011) 'Transfusion-transmitted Yersinia enterocolitica sepsis' in Clinical Infectious Diseases, 53(6), pp. 583-591.
Gupta, A., Yan, M. (2021) Transfusion-related acute lung injury (TRALI). Available at: https://professionaleducation.blood.ca/en/transfusion/publications/transfusion-related-acute-lung-injury-trali#:~:text=TRALI%20may%20be%20distinguished%20from,of%20TACO%20rather%20than%20TRALI. (Accessed 04/06/2025)
Heddle, N. (1999) 'Pathophysiology of febrile nonhemolytic transfusion reactions' in Current Opinions in Hematology, 6(6), pp. 420-426.
Imperial College Healthcare NHS Trust (2024) HLA typing (tissue typing). Available at: https://www.imperial.nhs.uk/-/media/website/patient-information-leaflets/childrens-services/childrens-haematology-and-stem-cell/tissue-typing-hla-typing.pdf?rev=31c177731aa94c969800986526a2f637 (Accessed 04/06/2025)
International Society of Blood Transfusion (2018) Transfusion-associated circulatory overload (TACO). Available at: https://www.isbtweb.org/static/19fed2c2-e257-42f5-9b2c2b51df1f87d4/TACO2018definitionMarch2019.pdf (Accessed 03/06/2025)
JPAC (2024) 7.1.1: Leucocyte depletion. Available at: https://www.transfusionguidelines.org/red-book/chapter-7/7-1/7-1-1 (Accessed 01/06/2025)
JPAC (no date a) Febrile non-haemolytic reaction. Available at: https://www.transfusionguidelines.org/transfusion-practice/consent-for-blood-transfusion/guidance-for-healthcare-practitioners-involved-in-this-role/febrile-non-haemolytic-reaction (Accessed 01/06/2025)
JPAC (no date b) Transfusion associated circulatory overload (TACO). Available at: https://www.transfusionguidelines.org/transfusion-practice/consent-for-blood-transfusion/guidance-for-healthcare-practitioners-involved-in-this-role/transfusion-associated-circulatory-overload-taco (Accessed 03/06/2025)
Kopolovic, I. et al. (2015) 'A systematic review of transfusion-associated graft-versus-host disease' in Blood, 126(3), pp. 406-414.
Latham, T. (2016) Transfusion-related acute lung injury (TRALI) n=o. Available at: https://www.shotuk.org/wp-content/uploads/2025/04/18a.-Transfusion-Related-Acute-Lung-Injury-TRALI.pdf (Accessed 04/06/2025)
Leeds Teaching Hospitals NHS Trust (no date a) Group and save. Available at: https://www.leedsth.nhs.uk/services/pathology/tests/group-and-save/ (Accessed 01/06/2025)
Leeds Teaching Hospitals NHS Trust (no date b) Crossmatch. Available at: https://www.leedsth.nhs.uk/services/pathology/tests/crossmatch/ (Accessed 01/06/2025)
Lifeblood (no date a) Acute haemolytic reactions. Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/acute-haemolytic-reactions (Accessed 31/05/2025)
Lifeblood (no date b) Febrile non-haemolytic transfusion reactions (FNHTR). Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/FNHTR#:~:text=Patients%20present%20with%20an%20unexpected,pressure%2C%20anxiety%20and%20a%20headache. (Accessed 01/06/2025)
Lifeblood (no date c) Minor allergic reactions (hives or urticaria). Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/minor-allergic-reactions (Accessed 01/06/2025)
Lifeblood (no date d) Severe allergic reaction (anaphylaxis). Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/severe-allergic-reactions (Accessed 01/06/2025)
Lifeblood (no date e) Transfusion-associated circulatory overload. Available at:https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/TACO (Accessed 03/06/2025)
Lifeblood (no date f) Transfusion-related acute lung injury (TRALI). Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/TRALI (Accessed 04/06/2025)
Lifeblood (no date g) Transfusion-associated graft-versus-host disease (TA-GVHD). Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/TA-GVHD (Accessed 04/06/2025)
Lifeblood (no date h) Transfusion-transmitted bacterial infection. Available at: https://www.lifeblood.com.au/health-professionals/clinical-practice/adverse-events/transfusion-transmitted-bacterial-infection (Accessed 04/06/2025)
Martins, J. et al. (2017) 'HLA and HNA antibodies are more prevalent in multiparous women with red blood cell alloimmunization' in Blood, 130(1), p. 3731.
NHSBT (no date) Frequently asked questions. Available at: https://www.nhsbt.nhs.uk/who-we-are/transparency/infected-blood-inquiry/frequently-asked-questions/ (Accessed 04/06/2025)
NICE (2015) Blood transfusion. Available at: https://www.nice.org.uk/guidance/ng24/chapter/recommendations (Accessed 01/06/2025)
North West Anglia NHS Foundation Trust (no date) Group & Save and crossmatch guide. Available at: https://www.pch-pathlab.com/cms/?q=node/328 (Accessed 01/06/2025)
Ontario Regional Blood Coordinating Network (2017) Patient fact sheet: special blood requirement- washed blood. Available at: https://transfusionontario.org/wp-content/uploads/2020/06/Patient-Fact-Sheet-Washed-Blood.pdf (Accessed 01/06/2025)
Oxford University Hospitals (2012) Blood transfusion policy and procedures. Available at: https://www.transfusionguidelines.org/document-library/documents/blood-transfusion-policy-and-procedures/download-file/rtc-scent_2015_06_P_tx_ox_univ_hosps.pdf (Accessed 01/06/2025)
Oxford University Hospitals (2015) Transfusion Laboratory: Frequently asked questions (Haematology). Available at: https://nssg.oxford-haematology.org.uk/nhsbt/files/transfusion-lab-faq.pdf (Accessed 01/06/2025)
Oxford University Hospitals (2024) The department of laboratory haemotology handbook V10.8. Available at: https://www.ouh.nhs.uk/media/oskntslv/haematology-handbook.pdf (Accessed 01.06/2025)
Papageorgiou, C. et al. (2018) 'Disseminated intravascular coagulation: an update on pathogenesis, diagnosis, and therapeutic strategies' in Clinical and Applied Thrombosis/Hemostasis, 24(9), pp. 8-28.
Resuscitation Council UK (2021) Emergency treatment of anaphylaxis: guidelines for healthcare providers. Available at: https://www.resus.org.uk/sites/default/files/2021-05/Emergency%20Treatment%20of%20Anaphylaxis%20May%202021_0.pdf (Accessed 01/06/2025)
Rout, P. et al. (2023) Hemolytic transfusion reaction. Available at: https://www.ncbi.nlm.nih.gov/books/NBK448158/ (Accessed 31/05/2025)
SHOT (2023) TACO pre-administration risk assessment. Available at: https://www.shotuk.org/resources/taco-pre-administration-risk-assessment-transfusion-associated-circulatory-overload/ (Accessed 03/06/2025)
SHOT (2024) Transfusion-associated circulatory overload (TACO) cumulative data. Available at: https://www.shotuk.org/resources/transfusion-associated-circulatory-overload-taco-cumulative-data-2/ (Accessed 03/06/2025)
Streiff, M. (2023) Disseminated Intravascular Coagulation. Available at: https://www.msdmanuals.com/professional/hematology-and-oncology/coagulation-disorders/disseminated-intravascular-coagulation-dic (Accessed 31/05/2025)
Suddock, J., Crookston, K. (2023) Transfusion reactions. Available at: https://www.ncbi.nlm.nih.gov/books/NBK482202/ (Accessed 01/06/2025)
Tobian, A. (2025a) Transfusion-associated circulatory overload (TACO). Available at: https://www.uptodate.com/contents/transfusion-associated-circulatory-overload-taco (Accessed 03/06/2025)
Tobian, A. (2025b) Transfusion-associated graft-versus-host disease. Available at: https://www.uptodate.com/contents/transfusion-associated-graft-versus-host-disease (Accessed 04/06/2025)
Williamson, L. (1998) 'Transfusion associated graft versus host disease and its prevention' in Heart. 80(3), pp. 211-212.





Comments